“It is as if all of my joints were locked and I am caught inside, as though imprisoned in a kind of body or an envelope that has padlocks inside, like doors that I cannot open.”
Fibromyalgia patient interview
(Valenzuela-Moguillansky, 2012)
Frustrating or fascinating – the complex world of Fibromyalgia Syndrome
Fibromyalgia Syndrome (FMS) can be one of the most challenging conditons to treat as a complementary therapist. Seemingly random and unrelated symtoms such as dizziness, aches, pains, sleep disturbance, ‘brainfog’, sore throat, heightened sensitivity and exhaustion are typical of the pathology And that’s just for starters! When you add into the mix the commonly co-related stress and mental health issues such as anxiety, depression and post traumatic stress disorder, you can see why the average therapist’s heart can sink a little at the prospect of successful treatment.

FIG 1 Fibromyalgia wordcloud
To make things even more complex, the delicate balance of the fibromyalgic conditiion means that it is not unusual for ‘normal’ massage treatment to result in increased pain and symptoms for the client.
Yet with a little knowledge and time, the well trained massage therapist can provide great relief for this complex conditon. The use of appropriate soft tissue techniques twinned with an understanding of the underlying psychological and physiological processes can bring about radical and long lasting change.
Fibromyalgia in a nutshell
In a nutshell, fibromylagia is a ‘syndrome’ – in other words a name given to a collection of symptoms. The symptoms can be endless (as we will see below) but in short, FMS can be mainly characterized by pain, fatigue, and sleep disruption.
FMS commonly exists with mental health and emotional issues including anxiety, panic disorder, post-traumatic stress disorder, and general depression.
Its prevalence in the general population is around 1%-2% and is more common in women (3.4% for women and 0.5% for men)
A ‘shopping list’ of symptoms

FIG 2 client care
The common symptoms of FMS are literally endless and can appear totally unrelated. Reading rather like a ‘shopping list’ of every nasty bodily and cognitive complaint you have ever heard of, the typcial FMS client is likely to experience a combination of symptoms including:
• Widespread constant pain in muscles, soft tissue and joints
• Painful and tender skin
• A feeling of burning, tingling, ripping
• Pins and needles
• Shooting pains
• Restless legs
• Numbness and fogginess
• Tender points in the body
• Trigger points – ‘knots’ in soft tissue that can cause referred pain
• A deep aching pain like toothache
• Pain that moves from week to week. Oten the client can’t identify exactly where the pain is
• Terrible stiffness
• Muscle weakness
• Nausea
• Giddiness, lack of balance, lurching, visual disturbances like blurring
• Dry eyes alternating with watering eyes
• IBS, constipation, diarrhoea
• Allergies and sensitivities
• Heightened sensitivity to light, sound, smell, touch
• Sensitivity to cold
• Constant low grade fever
• Tender lymph nodes in neck or arm pit
• Sore throat
• Increased sensitivity to pain(thought to be because of increase in substance P, a chemical that tells the brain that there is pain in an area)
• No energy, exhaustion, feeling wiped out all the time
• Feeling as if one has ‘flu
• Very long recovery time for any type of exertion
• ‘Disproportionate response’ to treatment and exertion; normal massage or deep tissue treatment will bring days of pain and inflammation; expending too much energy will result in days of not having any energy at all or not being able to get out of bed
• Anxiety
• Depression
• Irritability
• Mood swings
• Inability to sleep, or likelihood of waking up and not getting back to sleep
• Increased REM sleep and less deep restorative sleep, waking up feeling as if they have not slept at all
• Night sweats
• Brain fog – ‘fibrofog’, poor concentration, memory loss
The symptoms of FMS are so diverse it is common for sufferers to have spent months or years undergoing medical tests in an attempt to find a cause. This process in itself brings intense frustration for clients who may have been told that the symptoms are psychological or exaggerated – there is often an intense feeling of “not being believed” that clients carry around with them.
One big wind up – the importance of central sensitisation in FMS and chronic pain
So what is actually going on in this mysterious and debiliitating condition? FMS can be quite difficult to understand as although clients can be in terrible pain, there is no actual damage to any tissues or organs of the body.
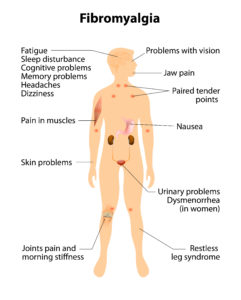
FIG 2 Fibromyalgia image
Central sensitisation has 2 main features: allodynia and hyperalgesia
• ‘Allodynia’ – This is when an neutral stimulus is interpreted by the brain as painful – for example, the stroke of a feather feels like being seared by a blowtorch.
• Hyperalgesia- a normally painful stimulus is interpreted as being much more painful
This explains why your client with fibromyalgia might be literally jumping off the treatment table when you are barely even touching them!
In addition, central sensitization can lead to heightened sensitivities across all senses including light, sound and smells and is associated with the cognitive deficits common to FMS such as poor concentration and short term memory. Central sensititization is also correlated with increased levels of emotional distress especially anxiety
It is vitally important when treating fibromyalgia to undersand that a main part of our job is to address this faulty and oversensitized alarm system.
Fibrmyalgia and Fascia: The missing link
FIG 4 – fascia
I always joke with my students that if they fall asleep in class and I ask them a question then the answer is most likely to be “fascia” (or “the psoas”). This is definitely the case with FMS as although no definite evidence of muscle pathology has been found, there is some evidence for dysfunction of the intramuscular connective tissue, or fascia, Research by Liptan (2010) proposes that inflammation of the fascia is the source of peripheral nociceptive input that leads to central sensitization in fibromyalgia.
Interestingly, the inflammation of the fascia is similar to that described in conditions such as plantar fasciitis and lateral epicondylitis, which also respond well to myofascial techniques.
Massage treatment for FMS
Treating clients with FMS can be challenging due to the extreme sensitivity of their systems. This means that every detail of the treatment process has to be thought through – from the smells in the room, to their positioning on the table, to the techniques and quality of your touch. Literally nothing can be taken for granted. Below are some top tips for working with FMS clients:
• Allow a good half hour for your initial consultation assessment and interview. FMS clients often have complex histories and it is vitally important that they feel truly heard
• Share your treatment plan: Tell them what you are doing and why and expect their input and comment.
• Be extra careful with basic client care. For example, have plenty of blankets ready, and have pillows to hand as basic positioning might be uncomfortable. Check in about temperature as your room might need to be warmer than usual
• Allow clients to change position often if they want. Staying in one position can be painful.
• Expect the tiniest amount of treatment to have a disproportionately enormous effect; don’t think you have to pack very much in to one treatment
• Remember the main issue in FMS is central sensitization – an over-reaction to threats. Treatment that is too intense may trigger the warning system and make things worse
• Listen to your client, take their word for everything they say. They really do know best. If they say ‘don’t touch my stomach’, DON’T!
• Keep treatments short if necessary, i.e. 20 – 30 minutes pain release at the most, follow with relaxation massage
• Be very, very gentle, light rather than deep. Find out each time which depth of weight is best for the client: what for us is felt as discomfort can be extremely painful to an FMS client
• With FMS you have to be prepared to be in it for the long haul. Progress can be very very slow over several treatments and often it doesn’t seem as if there has been much progress
Treatment techniques and tips
My own approach to treating chronic pain conditions has been developed through clinical practice with thousands of clients. For most chronic pain conditions including FMS, I recommend a multi modal approach incorporating several elements including the use of heat; fascial techniques, stretching, acupressure and self care suggestions.
A sample treatment for FMS could include the following:
The use of fascial techniques – Myofascial release without a doubt is the ‘go to’ technique for fibromyalgia. The cross hand stretch is one of my favourite MFR techniques and can be used anywhere on the body”

FIG 5 Cross hand stretch

FIG 6 Hot stones

Fig 7 Acupressure point CV 1
CV 17 is a wonderful point for helping to calm and release emotional energy
Conception Vessel 17 (CV 17) “Chest centre”
Location: On the sternum, level with the fourth intercostal space, between the nipples.
Use the third finger to hold the point for 3-5 breaths.
It feels nice to have the other hand under the head as you do this
Stretching – Gentle static stretching can be very helpful in areas of pain. The stretch shown is helpful for low back pain.

FIG 8 low back stretch for fibromyalgia
Self-care suggestions: Fibromyalgia clients often feel out of control so self help techniques that allow them some sense of empowerment are vital. Teach your clients gentle stretches and meditation/ breathing exercises for home care. Fibromyalgia is such a complex condition that a multi disciplinary approach works best for treatment. Referring your client to resources that can offer talk therapy such as CBT (cognitive behavioural therapy), gentle yoga, strength training or meditation will be extremely helpful in their recovery.

FIg 9 Selfcare for Fibromyalgia
Most of all, help your client to feel that there is hope. Recovery is certainly not quick but it is possible and as an understanding and well trained massage therapist you can be a key piece in this process.
Learn more with our MFR for fibromyalgia and post viral fatigue 1 day workshop
References
Liptan , GL J Bodyw Mov Ther. 2010 Jan;14(1):3-12. doi: 10.1016/j.jbmt.2009.08.003
About Rachel Fairweather and Jing Advanced Massage
Rachel Fairweather is author of the best selling book for passionate massage therapists – ‘Massage Fusion: The Jing Method for the treatment of chronic pain”.
She is also the dynamic co-founder and Director of Jing Advanced Massage Training (www.jingmassage.com), a company providing degree level, hands-on and online training for all who are passionate about massage. Come and take part in one of our fun and informative short CPD courses to check out the Jing vibe for yourself!
Rachel has over 25 years experience in the industry working as an advanced therapist and trainer, first in New York and now throughout the UK. Due to her extensive experience, undeniable passion and intense dedication, Rachel is a sought after international guest lecturer, writes regularly for professional trade magazines, and has twice received awards for outstanding achievement in her field.
Rachel holds a degree in Psychology, a Postgraduate Diploma in Social Work, an AOS in Massage Therapy and is a New York licensed massage therapist.
www.jingmassage.com
Tel: 01273 628942


Comments are closed.